Backtracking From Scleral Lenses: When Custom Soft Lenses Get the Job Done
by Priya Patel, OD.
Introduction
Scleral lenses provide significant visual and therapeutic advantages for patients suffering from a variety of corneal conditions: inclusive of kerato-ectasias, penetrating keratoplasties, and varying severities of corneal irregularities.
This advancement in the specialty lens realm has expanded to the use of sclerals, yet previous technologies are still capable of providing comparable comfort and vision.
Custom soft lenses have potential to significantly improve vision without the need for complex designs, and small diameter gas permeable lenses can achieve similar visual outcomes as sclerals at a fraction of the cost. Custom soft lenses can be entirely customizable from base curve, diameter, power, to even center thickness to improve upon masking corneal irregularities. Often in clinical practice, there exist simpler solutions to complex problems.
Case Report
A 46-year-old White male teacher with a history of keratoconus OD>OS presents to our office seeking scleral lenses. Patient JB has a history of gas permeable (GP) lens intolerance and has successfully avoided PKP (penetrating keratoplasties) in both eyes. The continuous irritation in his GP lenses and the fear they can pop out at any moment, has him seeking out scleral lenses.
His corneal shape shows most significant steepening directly over the visual axis, which would be well vaulted by a prolate design. Utilizing the Zenlens (Alden) Prolate fitting set, JB was fit into a 16.0 diameter scleral lens in both eyes, achieving BCVA 20/25 OD/OS. The initial fitting period was completed without any significant complications, and JB was happy to have clear, comfortable vision. At the one year mark after his initial scleral lens fitting, JB started to develop significant redness after 4 hours of lens wear with concurrent fogging, which only resolved after reinsertion of his lenses. After lens removal, the chronic irritation persisted. This led to intolerance of his lenses.
| Zenlens Prolate Scleral Lens |
Right Eye | Left Eye |
| SAG/Base Curve/Diameter (μ/mm/mm) | 4950/6.70/16.0 | 4950/6.70/16.0 |
| Power | -4.75-2.00×150 | -6.25-1.25×070 |
| Limbal Clearance Curve (LCC) | +60 | STD |
| Advanced Peripheral System | H = 7 steps flat V = STD |
2 steps flat |
| Visual Acuity | 20/25 | 20/25 |
JB became more frustrated, and he pleaded for any lens option, which would yield a similar visual outcome, but improve his comfort. We were sceptical we would be able to achieve this, but in an effort to exhaust all options available, we switched him into a custom soft lens modality in both eyes. To optimize comfort and reduce the chance of redness, fogging, irritation after lens removal as JB previously experienced, he is fit into the NovaKone Toric OD and Biofinity XR Toric OS. The custom soft lens selection was based on the poor BCVA (20/80+) attainable through refraction: the customizable center thickness of the Novakone lens would allow greater control in neutralizing irregular astigmatism in the right eye. The left eye was correctable to an adequate level (20/25+) with glasses so a monthly disposable lens had potential to correct JB to a level at which he would be functional.
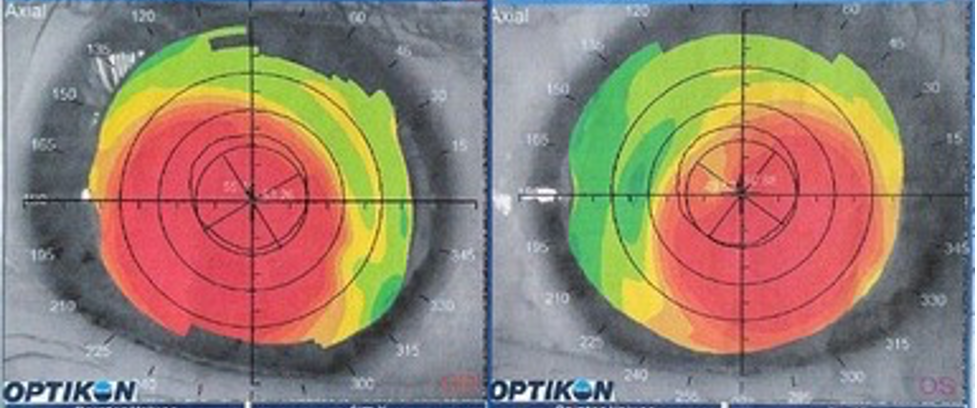
K Values:
OD: 55.15@121/53.26@031
OS: 50.88@053/49.52@143
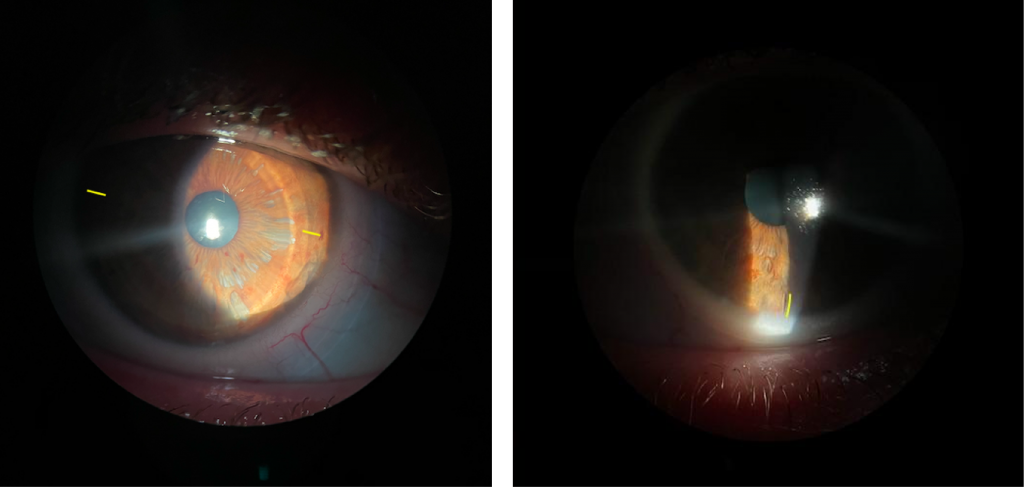
OD: Novakone Toric lens, rotated 15 degrees temporally (markings are highlighted with yellow dashes).
OS: Biofinity XR Toric lens, showing no rotation (lens marking is highlighted with a yellow dash).
| Refraction | |
| OD | -12.75-1.75×025 20/80+ |
| OS | -0.50-4.00×145 20/25+ |
| Custom Soft Lens | Right Eye | Left Eye |
| Name | Novakone Toric | Biofinity Toric XR |
| Base Curve/ Diameter (mm) |
7.8/8.4 IT=2 | 8.7/14.5 |
| Power | -7.00-0.75×020 | -2.00-2.75×160 |
| Visual Acuity | 20/20- | 20/20-2 |
These changes in lens modality improved his contact lens wearing experience and significantly simplified his daily lens wear routine. He has been in his new lenses for over a year with no degeneration in vision, and no recurrences of discomfort or irritation.
Discussion
Scleral lenses are a mainstay as a rehabilitative and therapeutic contact lens option, but alternatives exist for patients from mild to advanced cases of corneal irregularities. Taking into account comfort, lens handling capabilities, alternative specialty lens considerations can lead to improved outcomes as demonstrated in this case.
Scleral lenses require hand steadiness, ability for full control of fine motor skills, and neck mobility. Patients suffering from tremors, neck pain, or mobility issues often have trouble inserting scleral lenses on their own, but have minimal issues with soft and GP lenses. Improper insertion of scleral lenses can lead to air bubbles, and discomfort with lens wear. On the contrary, minimal risk is associated with difficulties with soft lens insertion .¹
Scleral lenses are associated with an increased risk of hypoxia if the tear film layer between the corneal surface and the back surface of the lens exceeds 200nm.²?³ Soft and GP lens lenses pose a lower risk for creating a hypoxic environment even for fragile corneas.
Utilizing higher modulus soft lenses allow some masking of irregular astigmatism for better visual outcomes. Although in this case, since JB achieved adequate vision through a refraction in his left eye, we were able to fit him in a lower modulus standard soft disposable lens. If he experienced difficulties with the quality of his vision in the left eye, a higher modulus monthly disposable lens would be his next option. His right eye, however, warranted a lens with a greater center thickness to mask his irregular astigmatism. Custom soft lenses are entirely customizable, inclusive of increasing the central thickness to enhance the masking of any irregularities.⁴
Scleral lenses will often be a superior lens for patients suffering from contact lens discomfort due to lens intolerance (without underlying dry eye disease). As they remain steady on the ocular surface, the optics can be decentered to allow for improved correction of higher order aberrations versus a soft lens or a GP lens.⁶
Conclusion
Soft contact lenses and gas permeable lenses are viable options for therapeutic lens correction. Scleral lenses can be considered an excellent choice as a troubleshooting lens, but it cannot be the only option available for patients who are seeking a specialty contact lens solution. When presented with a patient who is not comfortable in their scleral lenses, often a creative solution is warranted to find an alternative solution.
1. Fadel D, Toabe M. Scleral Lens Issues and Complications Related to Handling, Care and Compliance. JCLRS [Internet]. 2018Oct.26 [cited 2021Jan.13];2(2):e1-e13. Available from: http://www.jclrs.org/index.php/JCLRS/article/view/24
2. Compañ V, Oliveira C, Aguilella-Arzo M, Mollá S, Peixoto-de-Matos SC, González-Méijome JM. Oxygen diffusion and edema with modern scleral rigid gas permeable contact lenses. Invest Ophthalmol Vis Sci. 2014 Sep 4;55(10):6421-9. doi: 10.1167/iovs.14-14038. PMID: 25190661.
3. Michaud L, Vincent S. SCLERAL LENSES AND HYPOXIA: A BALANCED APPROACH. https://www.clspectrum.com/issues/2019/october-2019/scleral-lenses-and-hypoxia-a-balanced-approach. Published 2019.
4. Şengör T, Aydın Kurna S. Update on Contact Lens Treatment of Keratoconus. Turk J Ophthalmol. 2020;50(4):234-244. doi:10.4274/tjo.galenos.2020.70481.
5. Downie, L. E., and Lindsay, R. G. (2015), Contact lens management of keratoconus. Clin Exp Optom, 98, 299– 311. doi: 10.1111/cxo.12300.
6. Waleed Ali Abou Samra, Amani E. Badawi, Hanem Kishk, Ayman Abd El ghafar, Mohamed M. Elwan, Hossam Youssef Abouelkheir, “Fitting Tips and Visual Rehabilitation of Irregular Cornea with a New Design of Corneoscleral Contact Lens: Objective and Subjective Evaluation”, Journal of Ophthalmology, vol. 2018, Article ID 3923170, 8 pages, 2018. https://doi.org/10.1155/2018/3923170
Thank you to Dr Priya Patel for contributing to Global Insight.

Dr. Priya Patel received her Doctorate of Optometry from SUNY. She joined the premier practice in NYC and Long Island: Farkas, Kassalow, Resnick and Associates upon graduation, where she focuses clinically on speciality contact lens fittings. Dr. Patel routinely helps patients with keratoconus and other corneal disorders, as well as managing progressive nearsightedness with contact lenses (myopia management). She also designs and prescribes custom contact lenses such as scleral lenses, hybrid lenses, and multifocal lenses. Dr. Patel has authored articles in the area of specialty contact lenses, and hosted workshops on practice management related to specialty lenses. She is currently residing in London.