The Soft Lens Dropout Patient – Part 1
By Martin Conway
Could a “Soft Lens Dropout” be a potential patient for the Speciality Lens Practitioner?
Patient dropout and the reasons for it have long since been a subject of discussion within both the contact lens industry and profession. Speciality lens manufacturers normally supply lenses for patients who are perhaps more motivated than those who simply seek a cosmetic alternative to spectacles, therefore this topic doesn’t seem to be a subject for discussion at speciality lens meetings. The average keratoconus patient, for example, will tend to be more tolerant of occasional, or even constant, discomfort if the alternative is no vision and therefore no driving, no work and all that follows! As an industry, we have traditionally concentrated our efforts on supplying lenses that fall outside the range of mass-produced moulded lenses. High prescriptions, keratoconus, and other ectasia are our bread and butter. That market share, however, is gradually being eroded as the moulders extend their ranges and move into that space. More recently, myopia management associated with the use of ortho k lenses offered a boost to the speciality lens industry. With the use of ortho k lenses for children, a whole new arena opened up. The multinationals soon recognised the opportunity that this myopic pandemic presented, and we now have moulded, disposable options to compete within this growth market, and even spectacle lens manufacturers compete in this space. It might be wise, therefore, for us to take a look at the “Dropout” phenomenon that has plagued the disposable lens sector to see whether there is a potential market for a speciality lens solution for this perennial issue.
The “Dropout” Patient
Over the years, various studies have estimated the figure at anywhere between 18 and 30%. These are defined as patients that are supplied with lenses but drop out of lens wear at 6-12 months. I am convinced that a significant proportion of the supposed dropout figures consists of poorly motivated patients that were oversold the idea of contact lens wear as part of promotional activity in optical stores, so we should discount those, they were never really “in” to lenses in the first place. We really need to target those patients who would dearly like to have an alternative method of vision correction and who are prepared to put a little time and effort into attaining it. If those were just 25% of the dropout figures normally quoted, then that is a huge number for our industry. There have been many studies examining possible indicators that may predispose a prospective patient to be unsuitable for soft lens wear and although practitioners should conduct an evaluation of tear quality and associated functions before fitting a lens, little can be done to accurately predict the outcome until a lens is worn for a period of time. Indeed, if a practitioner were to try to advise a determined cosmetic lens wearer that they were unsuitable for lenses, they would probably simply find another practitioner. For a patient with an ectasia or ocular surface disease, it is easier to insist that they undertake some form of remedial action prior to commencement of fitting to improve tear quality and therefore improve both the experience and the chances of success in fitting. They consider this as part of their treatment process. A potential cosmetic wearer will still expect to try lenses for themselves, and although a practitioner might warn the patient of their concerns, most still allow the patient to evaluate some trial lenses for themselves, and provide an initial supply. These are future dropouts and our target market.
Case Study
Patient history
One such patient arrived in my clinic at Contamac recently and agreed to participate in a study. Natasha first tried lenses some ten years ago when she was in her late thirties, she is slightly myopic with no astigmatism and wants to be able to socialise, see at rugby matches, and wear fashionable sunglasses on holiday. As a receptionist, her low prescription (-1.00D) wasn’t an issue at work and around the home, so a supply of daily disposable soft lenses appeared to be the ideal option. Unfortunately, despite several attempts, she couldn’t tolerate them for more than 3-4 hours. This meant that at day-long social functions, such as a wedding, having to take them out after the photographs and wearing spectacles in the evening. Her last practitioner had correctly diagnosed a dry eye problem and left her with the impression that nothing could be done, and she might even cause damage if she were to wear lenses.

Case Studies are a regular feature in publications like Global Insight; normally they have been concluded and the practitioner is sharing their experiences with the benefit of hindsight. This case study will be slightly different in that it is currently in the beginning stages at the time of publications. At this stage, the outcome is not definite, and I propose to follow a course of treatment as the case unfolds and report findings along the way.
Initial Assessment
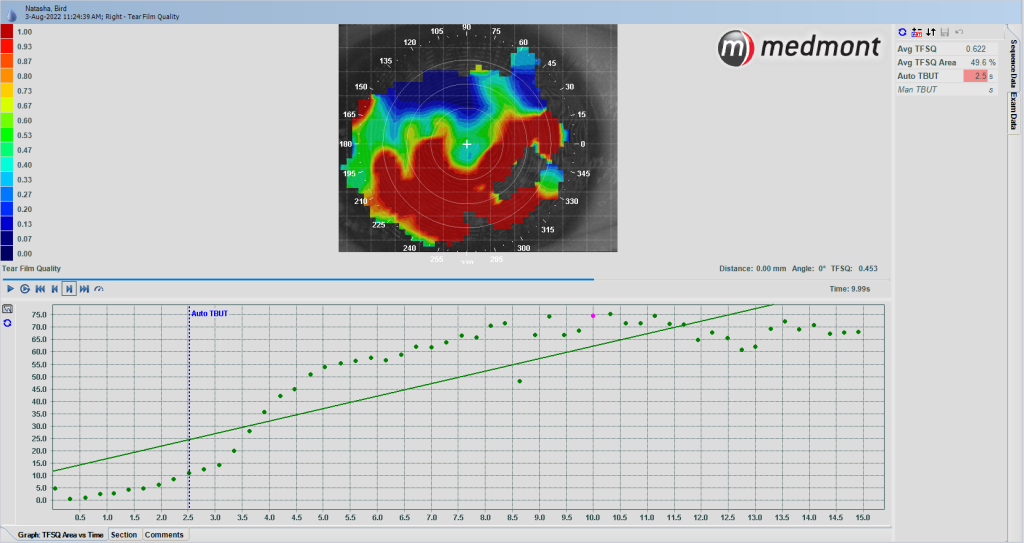
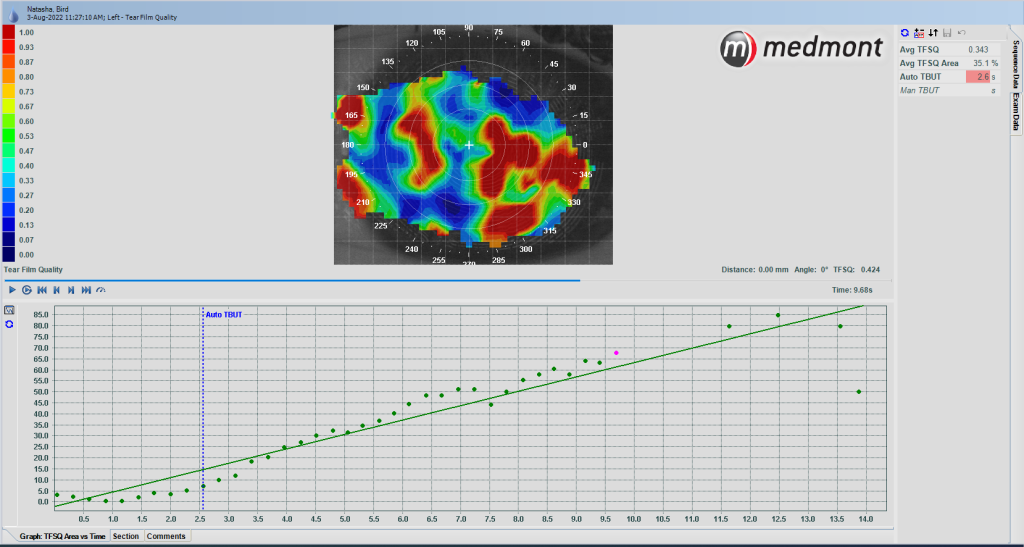
Fig 1 and 2: Non-Invasive Break-Up Time (NIBUT) Right and Left
I first decided to assess the scale of the problem. The Medmont has an excellent Non-Invasive Break-Up Time (NIBUT) feature and that measurement was a little concerning at 2,5 seconds for the right eye and 2,6 for the left! (Fig 1 and 2).
This feature is automatic and measures the time at which 25% of the visible tear film has broken up. The images show the tear film at the end of the process around 10 seconds when discomfort forced the patient to blink. With a NIBUT of 10 seconds being a “normal” measure, we can see the extent of the problem.
Lid margins showed no active infection, but some meibomian glands were blocked, (Fig 3).
Despite this, I ordered some hydrogel daily disposable lenses to be worn at work, so that I could monitor and observe fit, and get a measure of wearing time and, sure enough, at 3-4 hours they were irritating. Topography had shown the corneae to be on the flat side of normal, but otherwise, the fit was acceptable for the purpose intended.
Rather than simply try an array of different lenses as had previously been done, we agreed to try to improve tear quality as best we could before deciding upon the next course of action. Natasha is holding back one set of the trial lenses we had used for us to assess any improvement in wearing time and comfort once we have attained an improvement in tear break-up time.
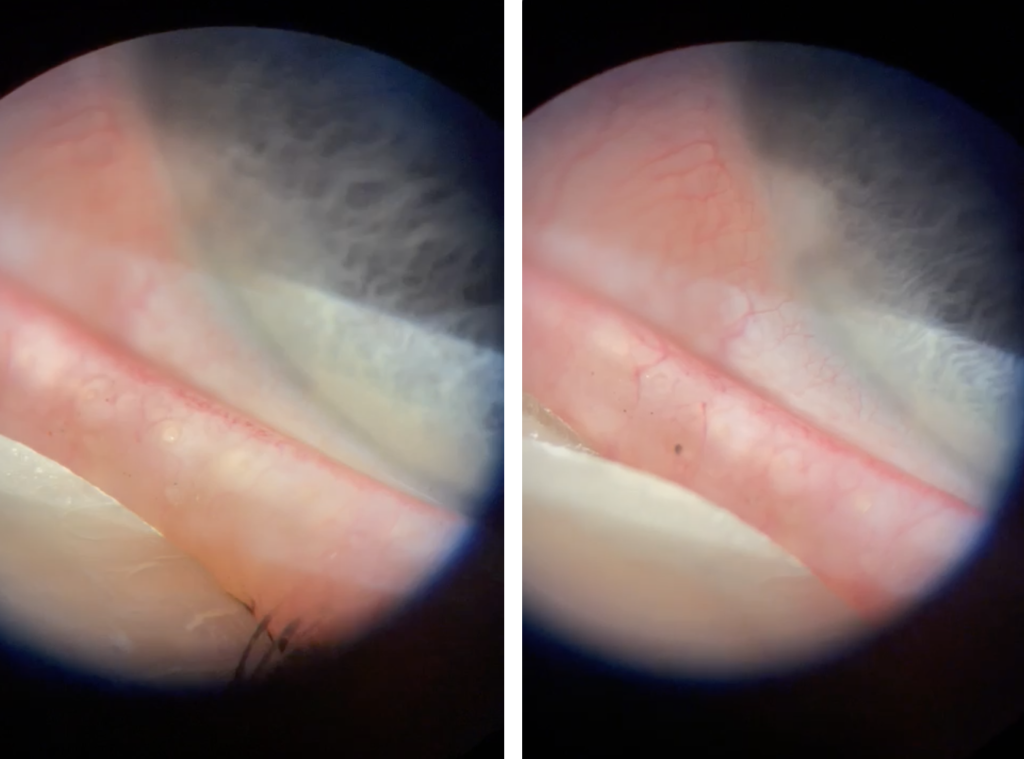
Fig 3: Meibomian gland assessment showed no infection but some blocked glands.
I am fortunate in that Natasha works here at Contamac, and is therefore readily available for consultations. She is also a willing volunteer and as interested in the progress of our investigations as I am. I appreciate that, in the real world, patients often demand an immediate result and will not necessarily be prepared to put up with the efforts required to improve tear quality and achieve a satisfactory result.
Speaking of results, I think at this stage it is important to set what is a realistic target for the patient. For Natasha, it is not to be able to become a full-time wearer of contact lenses. It is to be able to have to option to be able to go without spectacles for eight hours or so to attend the functions I mentioned earlier.
Treatment
Hot compresses, lid massage and lid scrubs will be the first stage. No active infection is present so no need for anything more complex at this stage. We’ll assess in a couple of weeks and decide on the next course of action. If the tear quality is sufficiently improved, I propose to try the same lenses as in the previous trial and see if the lid treatment has improved the comfort and wearing time.
Next Steps
I’ll report progress in the next edition of Global Insight and then in successive editions as the case progresses.
If you have any comments or suggestions either now or along the way, feel free to contact me and we can include those suggestions in the next edition.
Martin Conway has over 40 years’ experience in the contact lens field as a qualified Contact Lens Optician. He is registered with the UK General Optical Council on the Speciality Contact Lens Register. Martin is a fellow of the British Contact Lens Association (FBCLA), and The International Association of Contact Lens Educators (FIACLE). He has served in the Professional Services role as an educator and clinical adviser on behalf of both Sauflon and CIBA, and now acts as Professional Services Consultant for Contamac. Martin has lectured extensively in Europe, Asia, Russia, North and South America and the Middle East.
