Type 1 Lattice Corneal Dystrophy Status Post Penetrating Keratoplasty: A Scleral Lens Success Story
By Sharon Qiu OD MS
Background
Type 1 lattice corneal dystrophy (LCD1) is a rare hereditary bilateral disorder of the cornea. This is a result of an autosomal dominant mutation of the TGFBI (transforming growth factor beta induced) gene which leads to accumulation of amyloid deposits in stroma1
Variable clinical appearance depends on the stage of the disease2
- At the onset (usually by age 10): small filamentous anterior stromal lesions, mostly central
- With progression: lesions affect posterior stroma and opacify, eventually assuming a ground glass appearance throughout the cornea
- By the third decade: most patients will experience recurrent corneal erosions (RCEs) and reduced visual acuity (VA)
Diagnosis:
- Biomicroscopy examination alone is often sufficient to diagnose LCD1
- Corneal biopsy: can be used for definitive diagnosis3
Treatment: RCE management, phototherapeutic keratectomy and penetrating keratoplasty (PKP) in later stages3
Case Description – Patient MF
64-year-old Caucasian female, diagnosis of LCD1 OU confirmed by corneal biopsy with a corneal specialist.
Past surgical history
The patient had penetrating keratoplasty (PKP) OD in 2016, and cataract extraction (CE) OU (OD 2015, OS 2022).
Chief complaint
MF complained of blurred vision OU with PALs despite PKP OD, in addition to difficulty adjusting to new glasses since OS CE a few months prior.
Habitual glasses Rx with VA
OD -4.75-6.25×075 20/30- (PH 20/20-)
OS plano 20/50 (PH NI)
Add +2.50
Topography
OD tilted corneal graft with inferior elevation and steepening (Figure 1)
OS irregular astigmatism (Figure 2)
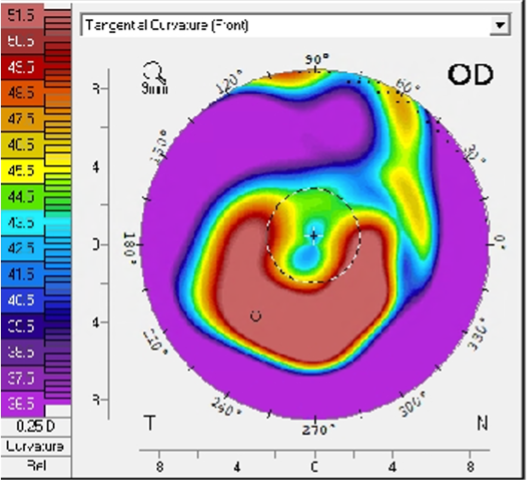
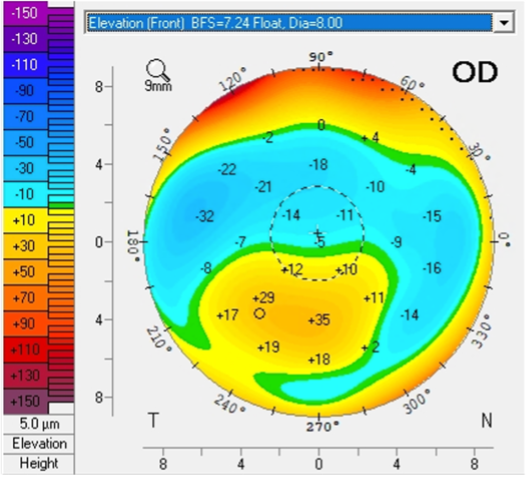
Figure 1: Topography of right eye at initial consultation visit
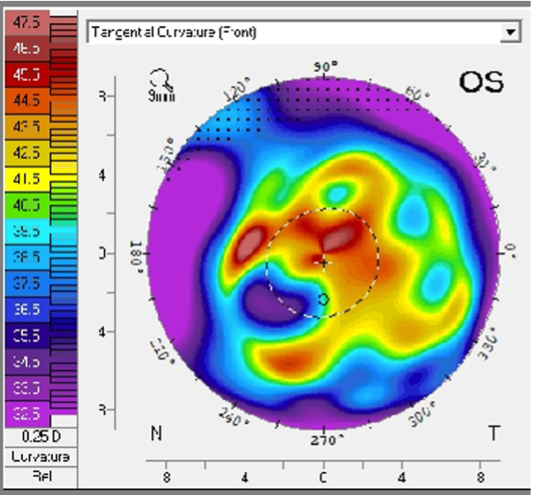
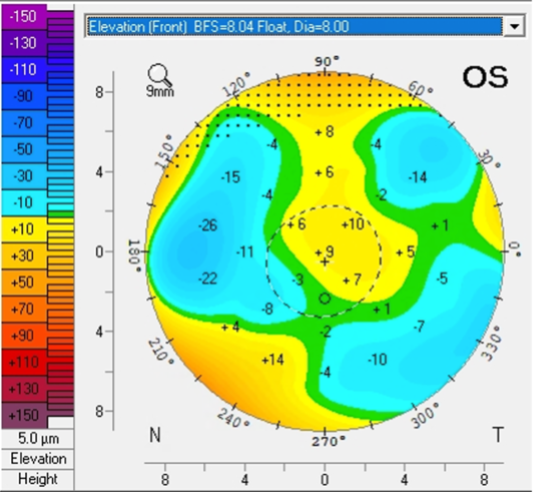
Figure 2: Topography of left eye at initial consultation visit
Slit lamp examination of cornea
OD: tilted corneal graft with inferior elevation, clear centrally (Figure 3)
OS: hazy ground glass-like lesions involving anterior and posterior stroma from limbus to limbus (Figure 4)
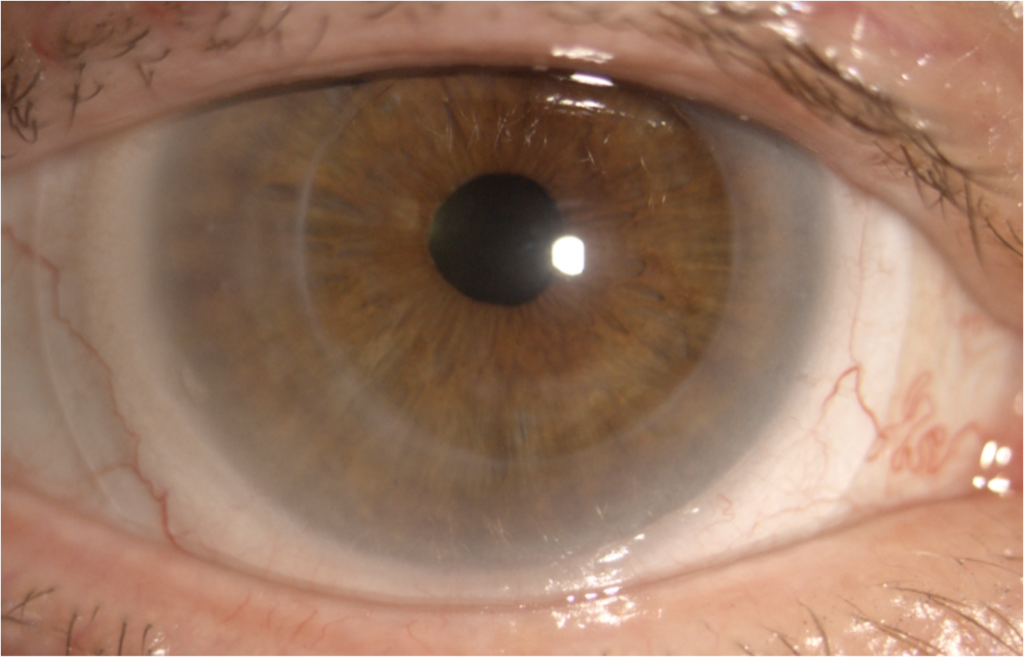
Figure 3: anterior segment photo of right eye wearing a scleral lens
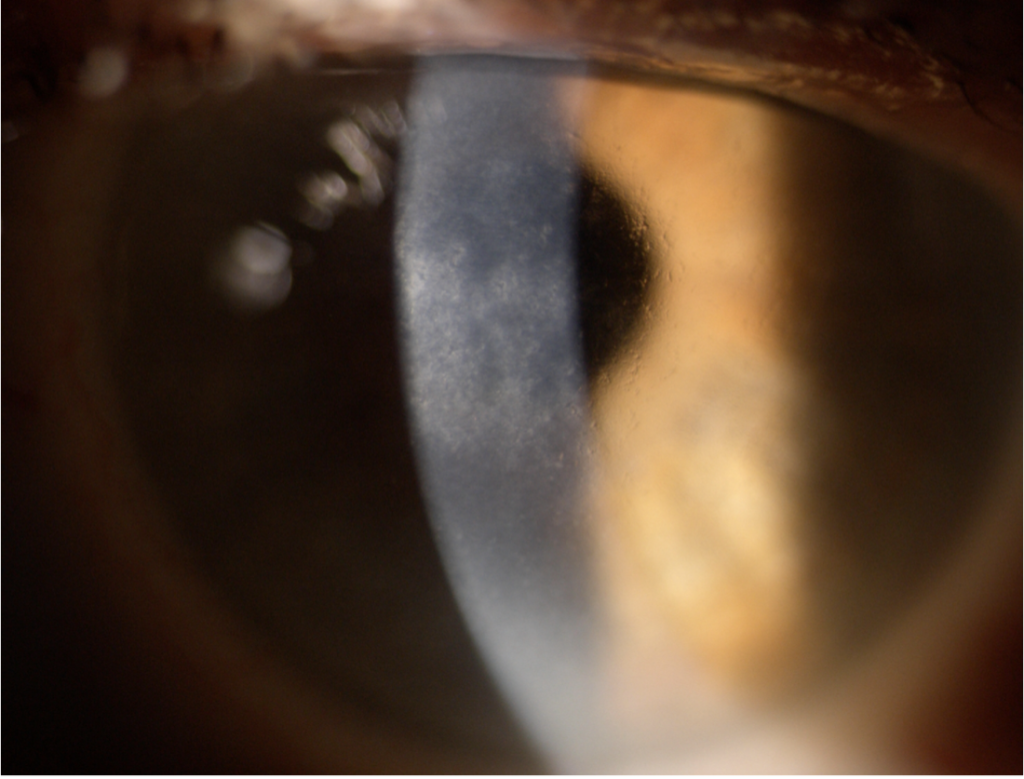
Figure 4: anterior segment photo of left eye showing lattice dystrophy
Scleral Lens Management OD
A Onefit MED scleral lens (Blanchard Contact Lenses) was ordered for OD only
Parameters
4300 / 7.78 / -5.37 / 15.6 / M-100 / L +25 / TPC +25/-125 / Optimum Infinite / 0.20
Two-week follow-up
BCVA OD: 20/20-
Excellent fitting relationship (Figures 5 and 6): central clearance of 210 μm after 4 hours of wear, good mid-peripheral and limbal clearance 360, edges aligned 360.
Patient reported clear and comfortable vision all day OD.
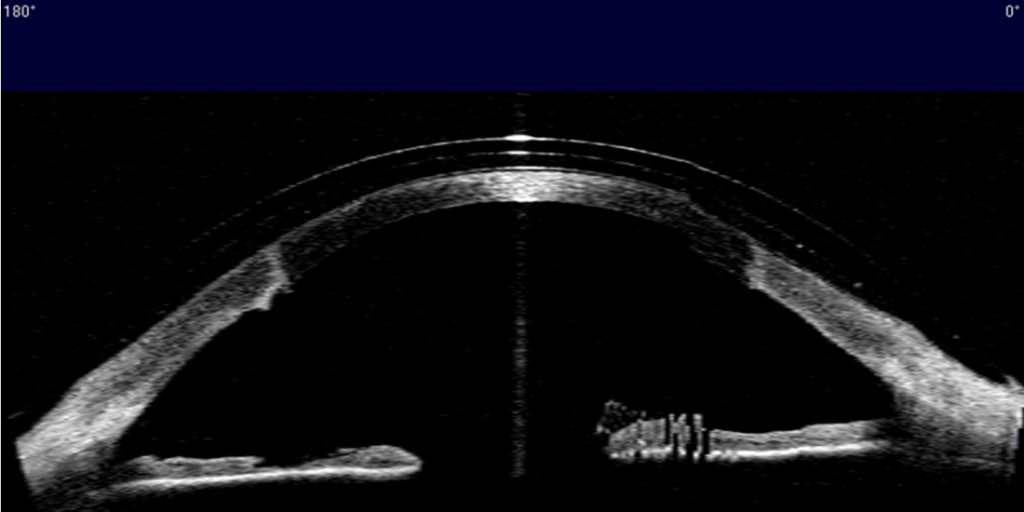
Figure 5: AS-OCT image of right eye wearing a scleral lens at two-week follow-up: excellent fitting relationship from limbus to limbus
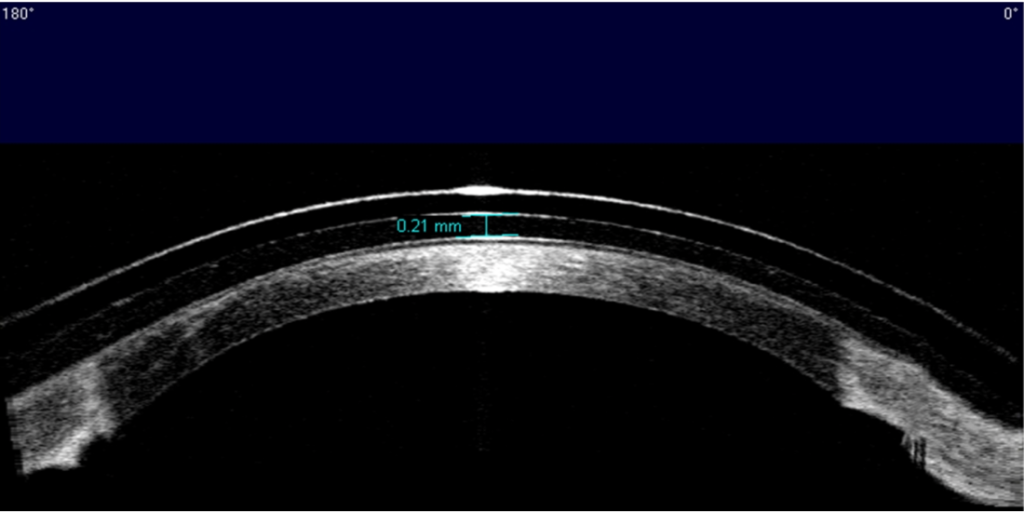
Figure 6: AS-OCT of right eye wearing a scleral lens at two-week follow-up: central clearance of 210 μm after 4 hours of wear
Discussions
For patients with advanced LCD1, scleral lenses can offer superior vision and comfort after PKP. Scleral lenses may improve vision in an eye with corneal dystrophy: significant improvement in BCVA (0.492 logMAR) in a study with 17 eyes with corneal dystrophy.4 However, patient MF was already considering having PKP done on OS before scleral lens fitting, due to having worse BCVA OS post-CE compared to pre-CE. When only one eye has undergone PKP, scleral lens fitting success in the post-operative eye can help accelerate the decision to operate on the other eye.
1. Afshari NA, Mullally JE, Afshari MA, Steinert RF, Adamis AP, Azar DT, Talamo JH, Dohlman CH, Dryja TP. Survey of patients with granular, lattice, avellino, and Reis-Bücklers corneal dystrophies for mutations in the BIGH3 and gelsolin genes. Arch Ophthalmol. 2001 Jan;119(1):16-22. PMID: 11146721.
2. Weis JS et al. The IC3D Classification of the Corneal Dystrophies. Cornea Volume 27, Suppl. 2, December 2008
3. Klintworth, Gordon K. Corneal dystrophies. Orphanet journal of rare diseases vol. 4 7. 23 Feb. 2009, doi:10.1186/1750-1172-4-7
4. Parra AS, Roth BM, Nguyen TM, Wang L, Pflugfelder SC, Al-Mohtaseb Z. Assessment of the prosthetic replacement of ocular surface ecosystem (prose) scleral lens on visual acuity for corneal irregularity and ocular surface disease. The Ocular Surface. 2018;16(2):254–8.

Sharon Qiu, OD, MS is a residency-trained optometrist with a passion for specialty contact lenses. She completed an OD/MS dual degree at the New England College of Optometry, where she graduated as the valedictorian of the Class of 2022. After graduation, Dr. Qiu completed a residency in Cornea and Contact Lenses at the University of Waterloo. Dr. Qiu is currently pursuing a full-time PhD in Vision Science at the University of Waterloo Centre for Ocular Research & Education (CORE). She is also serving as a part-time attending optometrist and supervisor for 4th year student interns at the University of Waterloo Contact Lens and Myopia Control Clinic. Her ultimate goal is to become a clinician scientist. She aspires to make a positive impact on her patients’ life, both at an individual level as a clinician, and at a global level as a researcher.
