Power profiles of Peripheral Additions using topographers with Soft Contact Lenses in Myopia Control
By Pascal Blaser and Ian Sexton, F.B.D.O. CL
Introduction
Various studies have demonstrated that both soft center-distance multifocal lenses and orthokeratology lenses are an effective option in myopia management. On average, the currently available standard geometries are shown to reduce myopia progression by approximately 50% (Data Walline JJ 2016, Figure 1).

Figure 1: Data from Walline JJ: MYOPIA CONTROL IN 2019; Contact Lens Spectrum March 2019
It is assumed that the effect of the contact lens periphery of both modalities perform the same function2. Currently, the most popular hypothesis for this effect of myopia control is the correction of hyperopic defocus on the retina through a relative myopic shift with peripheral addition in soft multifocals or the reverse zone of the orthokeratology contact lens (ortho-k). In another hypothesis, altered higher-order aberrations have a role to play3.
The majority of these studies were carried out using multifocal contact lenses, the monthly disposable Proclear® and Biofinity®, centre distance Multifocal lenses (CooperVision Inc.). However, these contact lens designs have been developed for presbyopic clients with relatively small pupils. It is known that pupil size reduce with age. The pupils shrink to approximately half their size from the second to the seventh decade of life (Benjamin WJ, 2006)4.
Chen et al. (2012) analyzed the influence of pupil diameter on the effectiveness of ortho-k in myopia control. His team concludes that a larger pupil diameter is more effective in slowing axial length elongation of the eye (nearsightedness). They presume that this can be traced back to an increase in myopic defocus in the retinal periphery5.
How do these multifocal lenses work and how do the power profiles of individually manufactured multifocal contact lenses impact the eye?
Topographic measurements of the eye, as well as power profiles, optical diameters, and the addition effect of the contact lenses were measured and compared using existing studies of peripheral defocus on the retina. Additionally, a case example compares the visual comfort with respect to different additions.
Methods
Contact lens measurements
A series of soft centre-distance focused multifocal contact lenses (Relax, SwissLens SA Switzerland), various additions and central optic zones (COZ) were measured on the eye with the Oculus Keratograph M3.
Additions of +1.50, +2.50, +4.00, +7.00, +9.00D with different central optic zone sizes were placed on the left eye, allowed to settle for 10 minutes, and measured with a topographer. The wearer was the same for all measurements, a person born in 1987 with a pupil diameter ranging from 3.5 mm (ambient) to 6.0 mm (dim). The contact lens parameters were 8.4/13.8 in GM3 58% (Contamac Ltd. UK). The base curve corresponds to the keratometry of the wearer’s cornea.
Case example
The contact lens was measured on the eye with the Oculus Keratograph 3 (Wetzlar, Germany) and is illustrated in the tangential view.
The example case was conducted on a 12-year-old Caucasian girl, voluntarily and with parental consent. The pupil diameter was measured to scale in room lighting (4.50 mm at 600 Lux) and dimmed room lighting (6.0 mm at 5 Lux and 5-minute adaptation time). The contact lens worn was identical to the one described above with a 4.50 mm COZ and additions of +1.50, +2.50, +4.00, and +7.00D. The visual acuity was measured with and without the respective contact lens in room lighting with 100% contrast and in dimmed lighting with 50% contrast (Essilor CS Pola 600).
Results
Topographic measurements of soft multifocal contact lenses on the eyes clearly illustrate their profiles. The effect of the addition and the diameter of the distance zone are both clearly visible.
Super elevated view
In Figure 2 (Relax) and Figure 3 (ortho-k), one can see the effect of both contact lenses in the super elevated power profile, and also identify that the profile of a -4.00D ortho-k correction is similar to a Relax lens with a +4.00D addition.
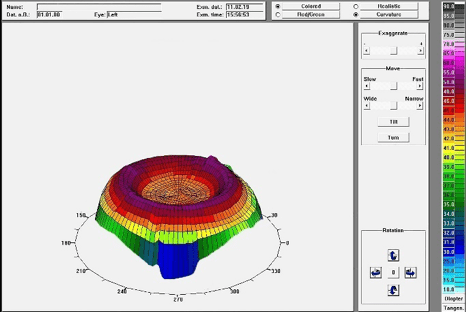
Figure 2: Superelevated view of the Relax with addition +4.00D, 4.5 coz on the eye
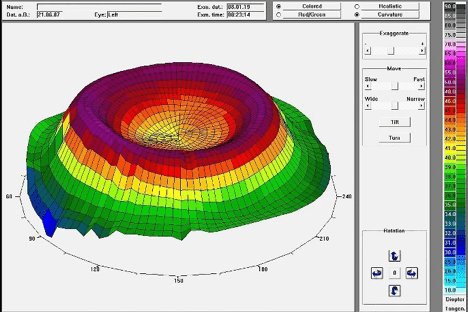
Figure 3: Superelevated view of NightFlex ortho-k with -4.00D correction
Figure 4 shows a soft multifocal contact lens with an addition of +1.50D. A lower elevation can be observed as opposed to that of the +4.00D addition in Figure 2. This addition of the contact lens has a correspondingly different effect on the eye.
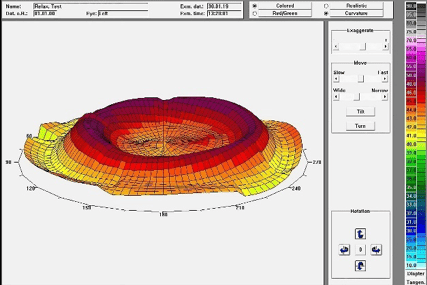
Figure 4: Superelevated view with Relax with addition +1.5D, 4.5 coz on the eye
Different strength profiles
Addition
It can be seen from the above that the power profiles of different additions in multifocal soft lenses closely match the topographical profile of the relevant ortho-k lens.
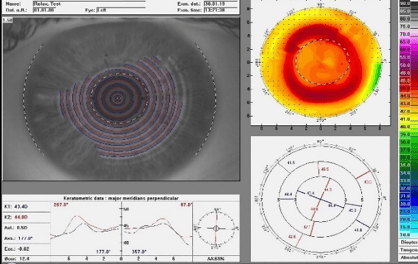
Figure 5: Relax topographic map with add +1.50, 4.50 coz
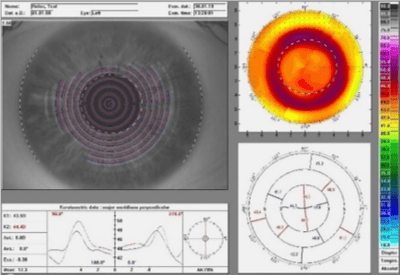
Figure 6: Relax topographic map with add +2.50, 4.50 coz
Figure 8 displays the topographic map of a cornea treated with ortho-k (-4.00D). Once again, the power profiles highly resemble the soft multifocal contact lens with a +4.00 addition from figure 7.
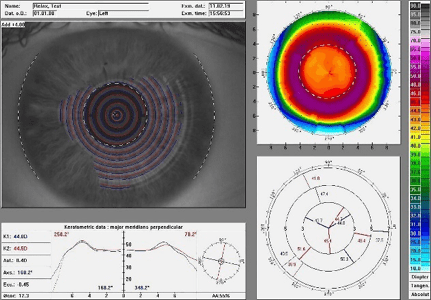
Figure 7: Relax topographic map with add +4.00, 4.50 coz
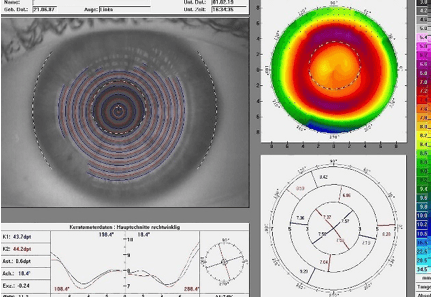
Figure 8: Cornea topographic map after ortho-k with -4.00D
Diameter
If the central optical zone of a multifocal contact lens changes, this alteration is transferred to the power profile on the topographic map and thus the addition location for the patient. Figures 6, 9, and 10 display the power profile with the same addition of +2.50D, but for different central distance zone diameters.
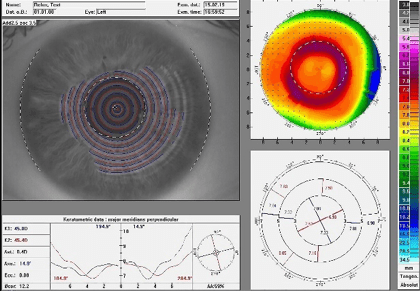
Figure 9: Relax topographic map with add +2.50, 3.50 coz
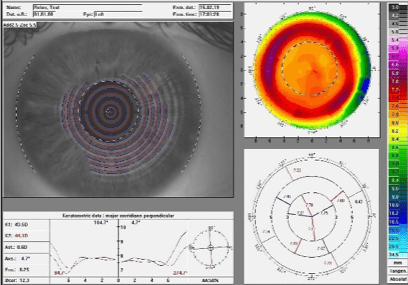
Figure 10: Relax topographic map with add +2.50, 5.50 coz
A patient with a smaller COZ will have a smaller distance range; the addition‘s effectiveness in correcting the peripheral defocus will, therefore, begin earlier in this case. Correspondingly, the distance range of use will be larger with a larger COZ diameter.
Differences in the peripheral image on the retina
Giancarlo Montani et al. have investigated different multifocal power profiles on their imaging on the retina and their correction of hyperopic defocus. They concluded that all additions and COZ‘s correct peripheral hyperopia according to their values (Figure 11), but the optical quality is affected by higher-order aberrations and different pupillary diameters (Figure 12)6.
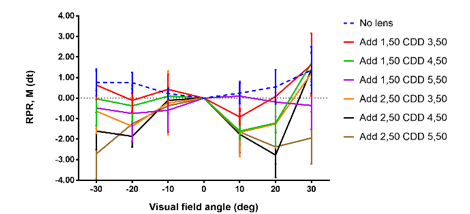
Figure 11: Montani G. et al. correction of hyperopic defocus with different additions and coz
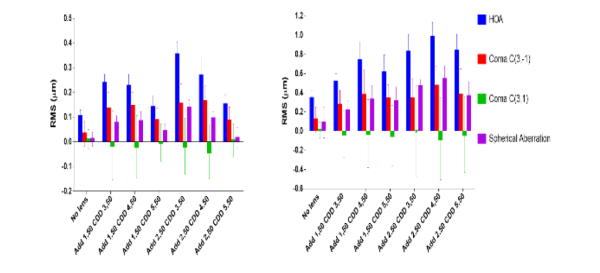
Figure 12: Montani G. et al. optical quality with different additions, coz and pupillary diameter
Example case
In the case of the 12-year-old child, the soft multifocal contact lenses were placed one after the other with an adaptation time of 10 minutes each. The distance visual acuity was measured in room lighting (600 lx) as well as in dimmed room lighting (5 lx).
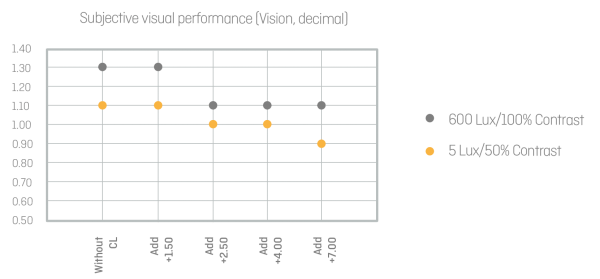
Figure 13: Evaluation of subjective visual acuity measurements of different strength profiles under 600 and 5 Lux
The results are similar to the data from the Comet Study7. The visual performance is barely differentiated with a low addition. The higher the addition, the lower the visual performance— particularly in low light conditions. With additions of +2.50, +4.00, and +7.00, the patient in the test subjectively identified double images in space. They were less visible in good lighting, and more clearly visible in lower lighting.
Discussion
Comparison with other products
Philip Cheng has published an article showing a topographic map of Misight®(CooperVision Inc. USA)8, and comparing this to Orthokeratology Misight® is a specially developed daily lens for myopia management with a multi-concentric optical design (Figure 14).
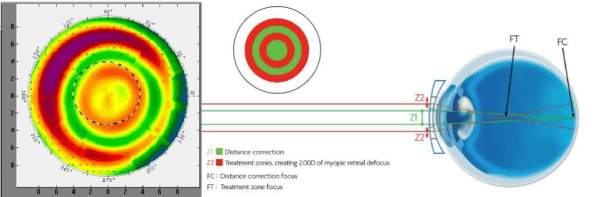
Figure 14: Structure and strength profile of Misight, CopperVision Inc. illustration https://coopervision.com.my/contact-lenses/misight/misight-activcontrol-technology
In this topographic map, one can identify the multi-zone principle which is typical of this contact lens.
When measuring the Proclear®/Biofinity® Multifocals with CD, the same strength profiles can be identified (Figures 15 and 16) as in the soft, Swiss Lens Relax contact lenses and similarly in Orthokeratology. Given that these contact lenses are designed for presbyopic patients, their distance zone is also smaller than in a standard ortho-k contact lens.
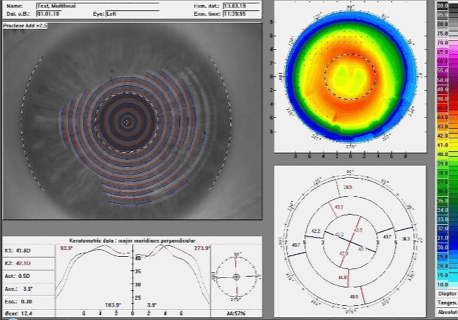
Figure 15: Strength profile of the Proclear multifocal add +2.50
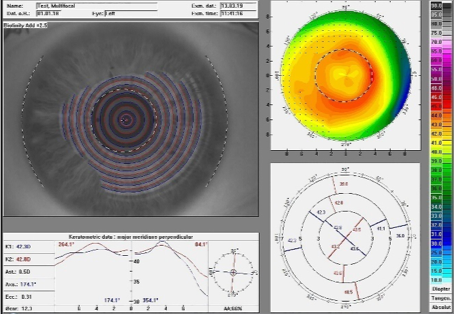
Figure 16: Strength profile of the Biofinity multifocal add +2.50
Use of topography in selecting the optimal periphery
With a topographic map of the lens, one can accurately identify the power profile and centering of the soft multifocal lenses. When comparing different designs of soft contact lenses with a topographic map of a cornea treated with orthokeratology, we can identify the similarity of the action. The peripheral addition of center distance multifocal contact lenses displays the same topographic map as a typical ortho-k pattern.
An optimal ratio between pupillary diameter, the addition and the size of the distance zone plays an important role in the success of myopia control, this includes both soft contact lenses and Orthokeratology.
Addition amount
The addition amount has relatively little influence on the visual acuity but has an effect on the optical quality. Whether the subjectively perceived double image may diminish through longer wear would have to be verified in a separate study. In his Article “Defining a Strategy for Myopia Control”, Langis Michaud et al. recommends +2.50D additions and higher for an effective shift of hyperopic defocus, but also points to a worsened contrast vision in lower light conditions9.
Recommendations
There is currently no evidence-based recommendation on the selection of contact lens parameters. Ideally, the peripheral strength profile in myopia control should be within the pupil, so that the addition and the distance zone can be large enough to allow for subjectively comfortable vision.
1. Walline, J. J. (2016). Myopia Control. Eye & Contact Lens: Science & Clinical Practice, 42(1), 3–8.
2. Walline, J. J., K. L. Greiner, et al. (2013). “Multifocal contact lens myopia control.” Optom Vis Sci 90(11): 1207-1214.
3. Wildsoet CF, Chia A, Cho P, et al. IMI – Interventions for Controlling Myopia Onset and Progression Report. Invest Ophthalmol Vis Sci.
4. Benjamin WJ, Borish IM. Borish’s clinical refraction. Philadelphia: W.B. Saunders; 2006.
5. Chen Z. et al. (2012) “Impact of Pupil Diameter on Axial Growthin Orthokeratology” OPTOMETRY AND VISION SCIENCE, 1040-5488/12/8911-1636/0 VOL. 89, NO. 11, PP. 1636Y1640
6. Giancarlo Montani et al. (2017) “Changes in relative peripheral refraction, HOAs and optical quality using a soft centre distance multifocal contact lens with different additions and optical zones.” Poster IMC 2017.
7. Fedtke et al. (2016): “Visual performance with multifocal soft contact lenses in non-presbyopic myopic eyes during an adaptation period” Clinical Optometry 2016:8
8. https://medium.com/mykidsvision/ortho-k-vs-multifocal-soft-contact-lenses-part1-8b2b2f4876ed
9. Langis Michaud; https://www.clspectrum.com/issues/2016/march-2016/defining-a-strategy-for-myopia-control
Thank you to Pascal Blaser and Ian Sexton for contributing to Global Insight.

Pascal Blaser is an optometrist from Switzerland and has an MSc in Vision Science and Business (Optometry). He is a member of the Board of Directors at EurOK and IAOMC, and is the Sales and Product Manager at SwissLens. His passion for myopia management led him to develop MyopiaCare, a standardised risk analysis questionnaire for short-sighted children and an information platform about myopia management for parents and eye specialists.
Ian Sexton has been a qualified Optician since 1990 and has been fitting complex contact lenses since 2000. Ian has worked in a large, UK based multiple optician, teaching professional and support staff how to fit contact lenses. Ian has also taught contact lens fitting at City, University of London, where he was responsible for teaching third-year undergraduate students. He is currently a Contact Lens examiner for the Association of British Dispensing Opticians, as well as Professional Services Manager for No7 Contact Lenses, a specialist manufacturer of RGP, soft and hybrid contact lenses.
Read more by Ian Sexton:
