Radial Keratotomy And Reverse Geometry Scleral Lenses
by David Foresto and Sandra Au
Case
ME, a 61-year-old lady, was referred to our practice for contact lens correction to improve the vision in the right eye. She had a history of right radial keratotomy (RK) in 1991, right retinal tear in 2015, and bilateral cataract surgery with YAG capsulotomy in 2019. Levels of refractive error prior to RK and cataract surgery were unknown.
ME reported blurred vision and polyopia in the right eye following cataract surgery even with spectacle correction.
Slit lamp examination showed right radial keratotomy incisions extending into the deep corneal stroma with no signs of corneal oedema or neovascularization. The patient had clear IOLs in both eyes. She had tilted myopic optic nerves and healthy maculae in both eyes.
Spectacle refraction was R -1.25/-1.00×180 (6/7.5) and L -0.25 (6/5).
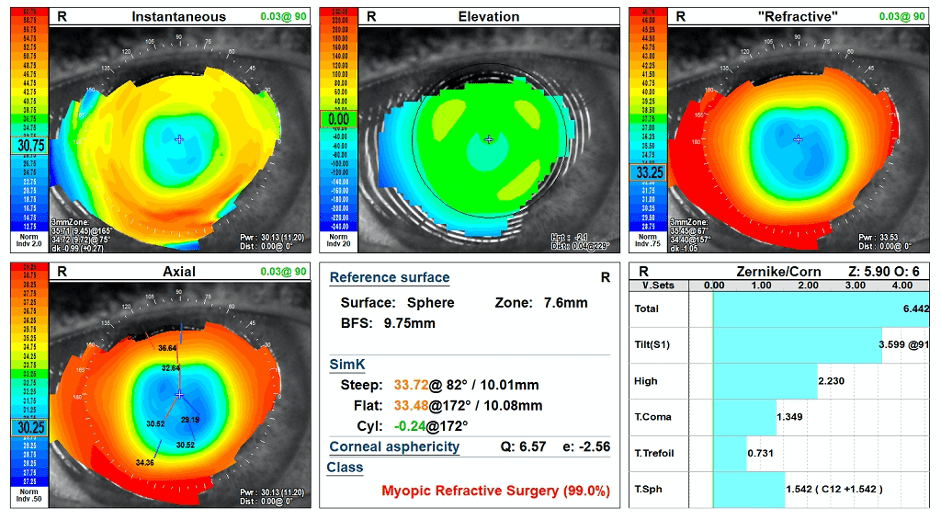
Corneal topography showed a very flat right cornea with mid-peripheral steepening. K readings were 10.01mm and 10.08mm. Whole eye aberrometry showed medium level higher-order aberrations in the right eye.
Refractive correction options were discussed and included updating her spectacles, fitting a soft contact lens or rigid contact lens. We decided to fit her with a rigid contact lens for optimal visual correction in the form of a mini-scleral contact lens to avoid touch to the cornea, improved stability and comfort. She did not require any contact lens for the left eye.
A reverse geometry design scleral trial lens with the following parameters was trialled:
8.28/15.0/+2.50 with Sag 4000 and 2.5D reverse curve.
There was a central clearance of 411um and an over-refraction of -16.50 (6/6-).
The lens was ordered with the following parameters:
9.0/15.0/-8.50 with Sag 3900 and 5D reverse curve.
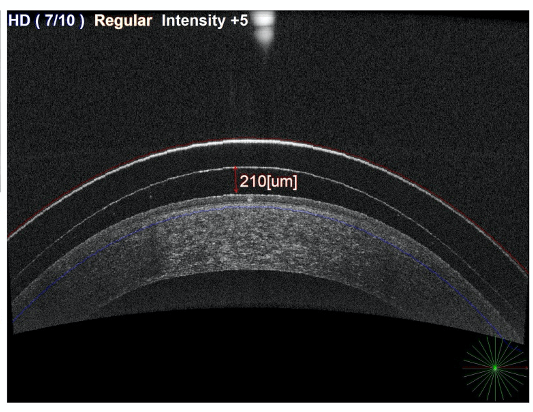
The patient achieved 6/6 vision and there was a central clearance of 210um and good limbal clearance. The lens material was Optimum Infinite with Tangible Hydra-PEG surface treatment for supreme oxygen and wettability.
ME was very happy with the visual outcome and comfort of the scleral contact lens. She no longer experienced symptoms of blur, haloes or polyopia.
Discussion
Radial keratotomy (RK) was first performed by Russian surgeon Professor Svyatoslav Nikolayevich Fyodorov in 1974 and was popular to correct myopia up until the late 1980s. This surgical technique involved making corneal incisions in a radial pattern, like the spokes of a wheel, to reduce the strength of the peripheral cornea. The intraocular pressure of the eye would cause steepening of mid-peripheral cornea leading to a relative flattening of the centre of the cornea. The number of incisions could range from 4 to 16, with the centre 4mm of the cornea spared.
There are various complications associated with RK which can occur early on or late. Complications related to visual outcome include unstable refraction with a tendency to progressive hyperopia, diurnal fluctuation of vision, irregular astigmatism, increased glare and reduced contrast sensitivity.
Other complications include progressive ectasia, corneal perforations, endothelial damage, increased risk of infection, and incisional neovascularization. Sometimes the complications can lead to the need for a full-thickness corneal transplant.
Often spectacle correction is not adequate due to large anisometropia between eyes, irregular astigmatism, higher-order aberrations, and monocular polyopia. In the past, hydrogel soft contact lenses were not suitable as they caused hypoxia and incisional neovascularization. Silicone hydrogel lenses with high oxygen permeability and flatter base curves are sometimes a good option if there is minimal astigmatism and fit the cornea adequately without buckling or fluting. However diurnal fluctuations in vision may not be corrected by the soft contact lens.
Rigid contact lenses provide best visual outcome and practitioners should generally use a reverse geometry design due to the oblate cornea. When fitting scleral contact lenses for compromised corneas such as RK, there is further emphasis on ensuring high oxygen transmission to avoid hypoxia and incisional neovascularization. This includes avoiding excessive clearance as a larger tear layer will reduce oxygen transmissibility. It is important to use a contact lens material which is hyper Dk; the selected material, in this case, was Optimum Infinite, coated with Tangible Hydra-PEG surface treatment.
Fitting contact lenses for patients with RK can be challenging, however with the development of reverse geometry lens designs and hyper Dk materials, excellent comfort and vision can be achieved without further compromise to the cornea.
Thank you to David Foresto and Sandra Au for contributing to Global Insight.

David Foresto is an Australian optometrist and contact lens practitioner specialising in contact lens fitting for keratoconus, corneal grafts and paediatric aphakia. David is a visiting lecturer at the Queensland University of Technology School of Optometry and a former President of Optometry Queensland/Northern Territory.

Sandra Au graduated from the Queensland University of Technology School of Optometry. She has a special interest in glaucoma and contact lenses, and enjoys mentoring students as a clinical supervisor at the Queensland University of Technology.
Related Case Studies:
